Timeline
2 months
June – August 2017
Context
Hospitals frequently need to give medications to patients that could cause serious problems if something were to go wrong – think opioids, narcotics, insulin, anything that’s dangerous out-of-the-box. Nurses have to be very careful when administering such dangerous medications to patients. That’s why hospitals have a special protocol for handling them, calling them “High Alert” or “High Risk” medications.
Most hospitals require that a second nurse validates and co-signs the administration. In order to do so, this second nurse is in the room with the nurse who’s administering the medication to make sure that everything is being done properly. After overseeing the administration, the second nurse co-signs it as part of an audit trail that would be pulled up in the event of an accident or lawsuit.
It’s crucial for the Medication Administration Record (MAR) – the workflow where nurses document what they give to patients – to support proper documentation of high alert medications. Without proper support, the MAR might unintentionally lead nurses to break protocol. Not only would this be a huge patient safety issue, but it’d be grounds for legal action against the nurse and/or hospital.
Problem
I need to be able to quickly locate high alert medications on the MAR.
Nurses need to know if they need to find another nurse to be in the room with them. We decided to explicitly call out High Alert medications on the surface of the MAR.
A second nurse needs to validate my work with a co-signature.
The validating nurse needs to sign their credentials on the administration task. We decided to call out tasks that need validation. It’s crucial that the validation is tied to the validating nurse’s user account for clear auditing and malpractice prevention.
Documenting and validating the administration happens in real-time when the patient is receiving the medication, but documenting the validation happens once the administration work is done.
Documenting the validation shouldn’t block documenting the administration. We designed the workflow to avoid this blocker.
Process
Identify User Stories and Goals
The first step of the process was identifying the nurses’ key steps in the High Alert medication administration workflow. We interviewed clients as well as internal nursing and patient safety subject matter experts, and read up on hospital policies and regulations to make sure that we had a comprehensive understanding of these high risk scenarios.
We also gathered feedback on the existing High Alert workflow in the old MAR to learn what worked well and what could be improved.
Our key findings were:
- During a High Alert medication administration, there are two nurses and only one computer – even though the nurses work together in real-time, they can’t both document in real-time
- The most critical information to document is what was administered – documenting the validation can wait if it must
Understanding Boundaries
During our research, we learned that some of our competitors’ MAR solutions allowed for the validating nurse to enter their credentials directly into the MAR to sign their validation. We looked into whether or not this was possible for us to do, and after talking with our back-end security team, we learned that it wouldn’t be possible, at least not in the near future. This locked us into a solution where the validating nurse must login separately from the administering nurse’s session.
In talking with our clients and looking at their databases, we found that a lot of our clients weren’t using the existing High Alert workflow – that means that they weren’t classifying opioids, narcotics, insulin, etc. as High Alert in their drug formularies. Not only is that very dangerous for their patients, but it’s also a compliance violation. They did this "workaround" because the High Alert workflow took too long (more on that in a moment).
I have to hand it to our clients – they could be very clever. We found that Pharmacists were typing "***HIGH ALERT***" into the order’s note field during Pharmacy Verification so that nurses would see that on the MAR. Not only was there risk that the nurse wouldn’t see that note, but they were also sidestepping a serious safety protocol by not classifying dangerous medications in their formularies. Based on this, we knew that we had to make serious improvements to the High Alert workflow.
High Alert in the Real World
Let’s take a look at how High Alert medication administration works in real life and compare it our workflows. N1 is the administering nurse; N2 is the validating nurse.
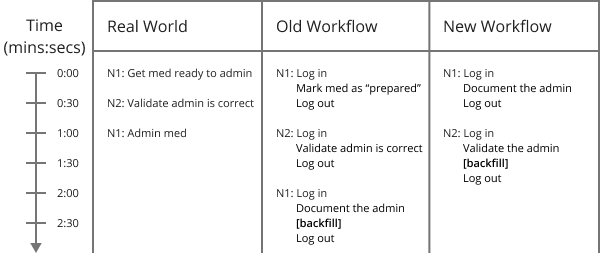
Due to the physical disconnect between the computer and the real world, information has to be backfilled at some point. It’s safer to backfill a validation than it is an administration because of how much more information needs to be entered or remembered for an administration.
Also, Nurse 2 is primarily validating that the patient received what they were supposed to be given. Validating that Nurse 1 got everything ready correctly comes second to that.
The old workflow required the administering nurse to log in twice and set “preparation” validation (a concept that doesn‘t translate perfectly into the real world) as a blocker to the documentation of the administration. These things frustrated users and consumed so much of their time that they would either backfill their administration documentations or have their Pharmacist turn off the High Alert workflow.
The new workflow eliminated that second log in for the administering nurse by removing the “preparation” step altogether to better match the real world. It also removed the blocker to administration documentation, a change that eased users’ frustrations.
Final Design
The design approach for the High Alert med workflow was strictly driven by qualitative and quantitative data. By the time this workflow bubbled up to the top of our backlog, we had already defined most of the interface elements in the new MAR, so we utilized them to our advantage.
The “North Star” vision for this workflow was to have a validation task assigned to a specific nurse and appear in their inbox for them to sign. We didn’t have enough time to build and coordinate all of that, so we needed a way to call out that a task needed its validation to be documented in the MAR.
We iterated through several different design options and got feedback on them, but I’d like to focus on the final result. Here is a step-by-step walkthrough of the workflow:
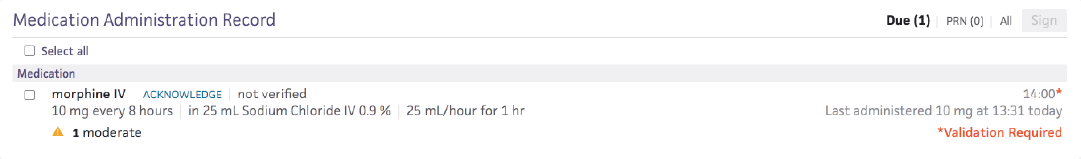
1. Administering nurse (N1) logs in and navigates to their patient’s MAR
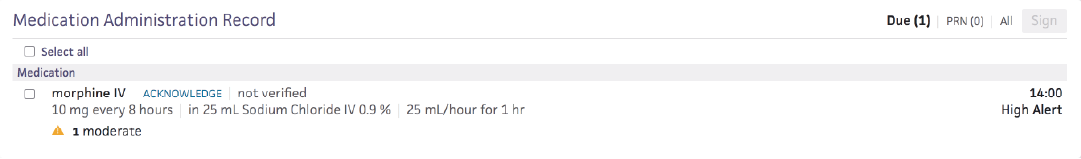
2. N1 documents the administration
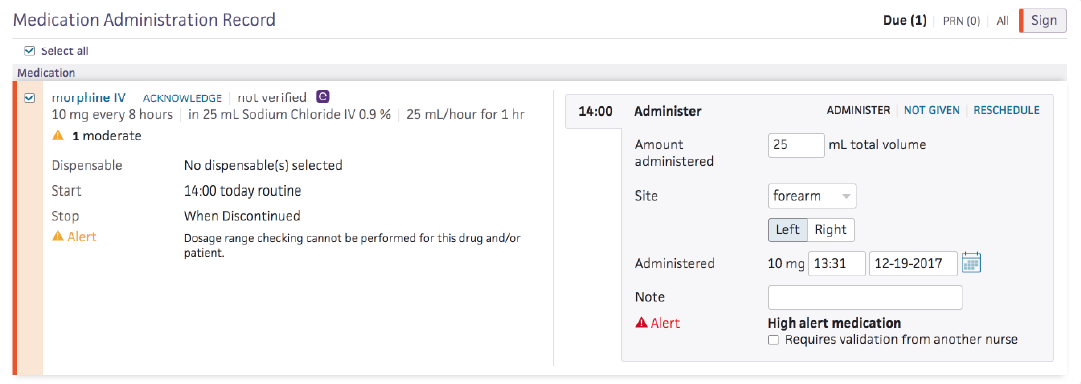
3. N1 must acknowledge that this medication is High Alert
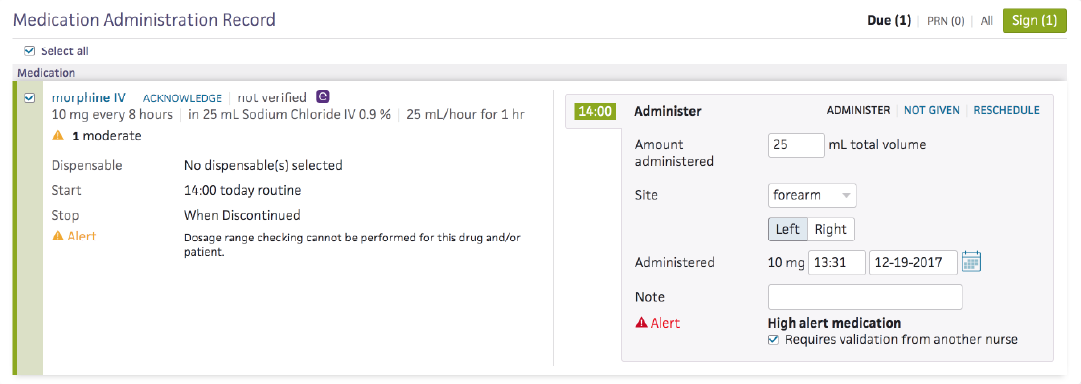
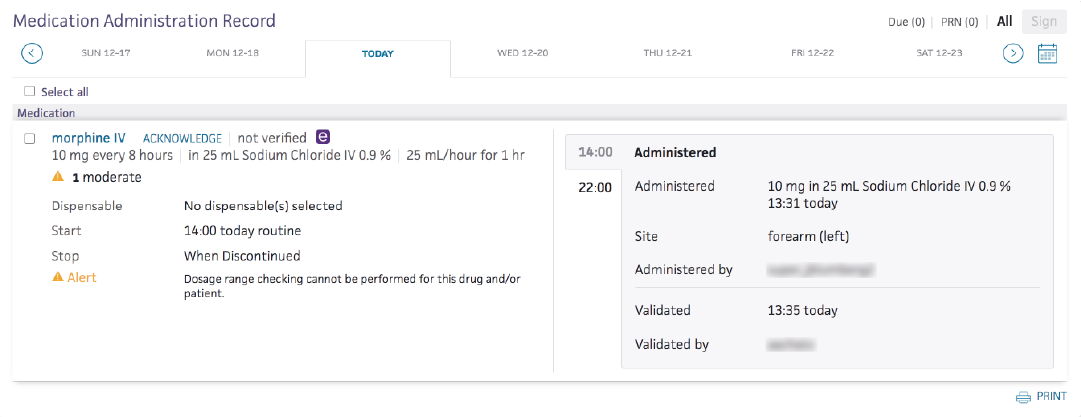
4. N1 signs administration and logs out. Validating nurse (N2) logs in and goes to MAR
5. N2 expands the order to view the task requiring validation
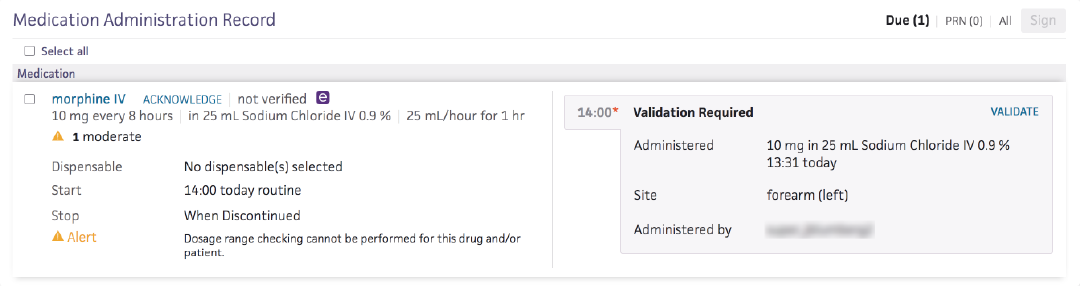
6. N2 clicks the “VALIDATE” action link to launch validation documentation
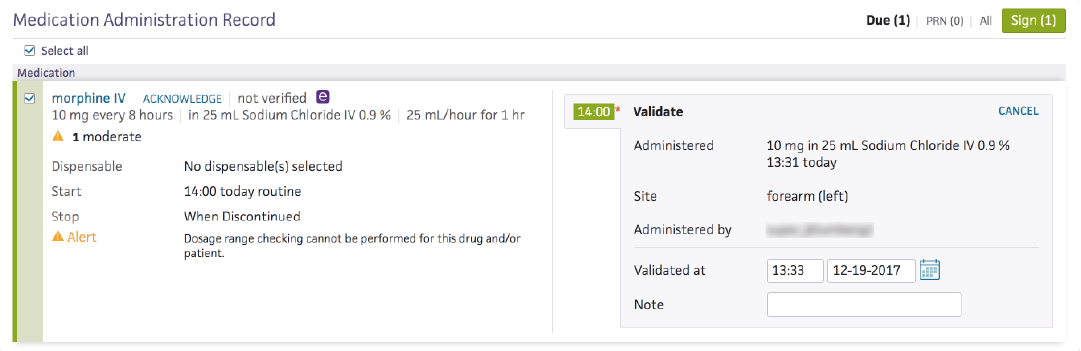
7. N2 signs validation and navigates to the All tab to view historical tasks
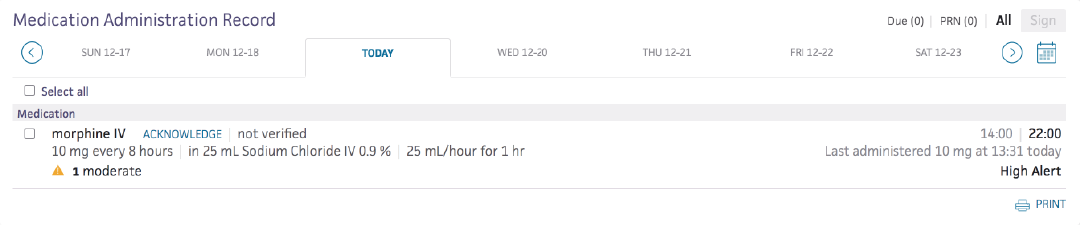
8. N2 expands the order to view the validation information
Quantitative Business Impacts
We did a speed test of the old High Alert workflow vs. the new one and found that on average, the new workflow was ~60% faster.
Biggest Takeaways
- Understand your constraints and boundaries so that you can plan for them ahead of time
- Use conventions that have been established in the consumer marketplace to your advantage (e.g. use of asterisks)
- If a workflow can’t perfectly match the real-world scenario, make sure the differences don’t get in the way